Steps in the Claim Submission Process
1. Patient Registration
All begins with registering the patient. This includes gathering:
Personal details
Insurance coverage
Medical and financial history
2. Determining Financial Responsibility
Not all services are fully covered. The patient may owe a portion of the cost. Clear communication at this stage avoids confusion later and ensures the patient understands any out-of-pocket expenses.
3. Medical Coding
Once treatment is provided, a professional coder translates the services and diagnoses into ICD-10 and CPT codes. These codes are essential for accurate billing and determining reimbursement amounts.
4. Superbill Creation (for Out-of-Network Providers)
For patients seeing a provider outside their insurance network, a superbill is created. This document summarizes the patient’s visit, codes and services, forming the basis of the claim.
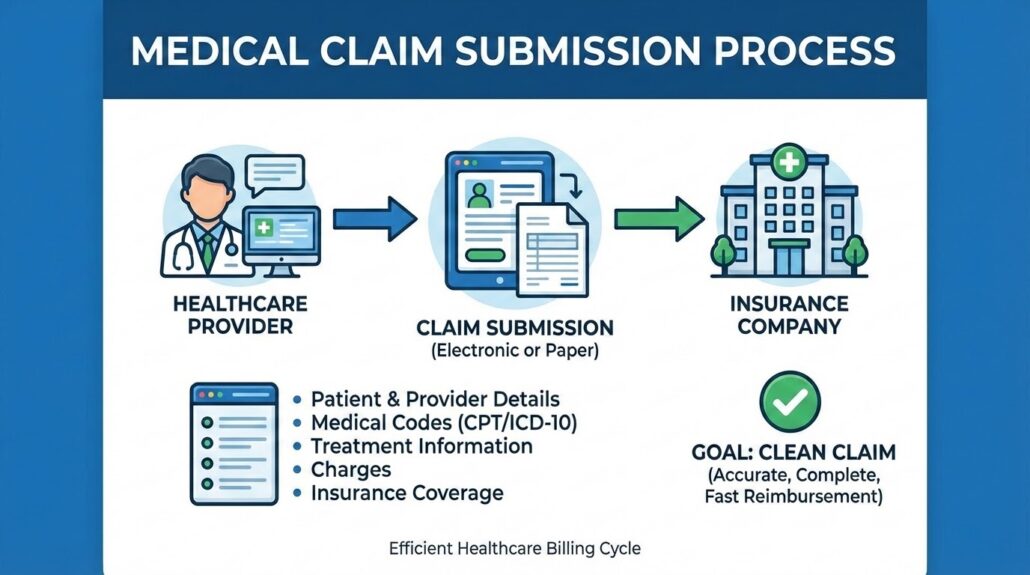
5. Claim Preparation & Submission
The claim is carefully prepared, reviewed for errors and submitted to the insurance company. Common forms include CMS-1500, UB-04, and ADA Dental forms. Clean submissions are processed quickly, while errors may trigger denials.
Methods of Claim Submission
Electronic Submission: Fast, secure, and efficient. Most providers now submit claims electronically through clearinghouses.
Paper Submission: Slower and more error-prone, but still used in some cases, especially for providers or insurers that don’t support electronic submissions.
Common Reasons for Claim Denials
Even with careful preparation, claims can be denied. Some common reasons include:
Incorrect or incomplete patient information
- Late submission beyond the insurance deadline
- Errors in coding or billing
- Services not covered under the policy
- Treatments deemed unnecessary
- Pre-existing conditions not covered
- Expired insurance policy
- Lack of required pre-approval
- Duplicate claims
- Claims lost by the insurance company
Best Practices for Clean Claim Submissions
Verify Patient Information: Double-check demographic and insurance details.
Accurate Coding: Use the latest CPT and ICD-10 codes.
Timely Submission: File claims promptly to meet deadlines.
Follow-Up: Track claims and address any rejections immediately.
Documentation: Keep thorough records to support the claim.
Why Claim Submission Matters
A smooth claim submission process ensures:
Timely reimbursement for healthcare providers
Accurate payments from insurers
Reduced financial burden on patients
Operational efficiency for medical practices
Legal & Regulatory Considerations
HIPAA Compliance: Protects patient privacy during electronic or paper submissions.
Fraud Prevention: Regular audits help detect and prevent fraudulent claims.
Conclusion
Medical claim submission is the backbone of the healthcare billing process. Understanding it thoroughly from patient registration to coding, claim creation and submission can dramatically improve reimbursement outcomes.
Even small improvements in the accuracy and quality of submissions can save practices time, money and headaches. For healthcare providers and billers alike, mastering this process is essential for a smooth, efficient and financially stable practice.