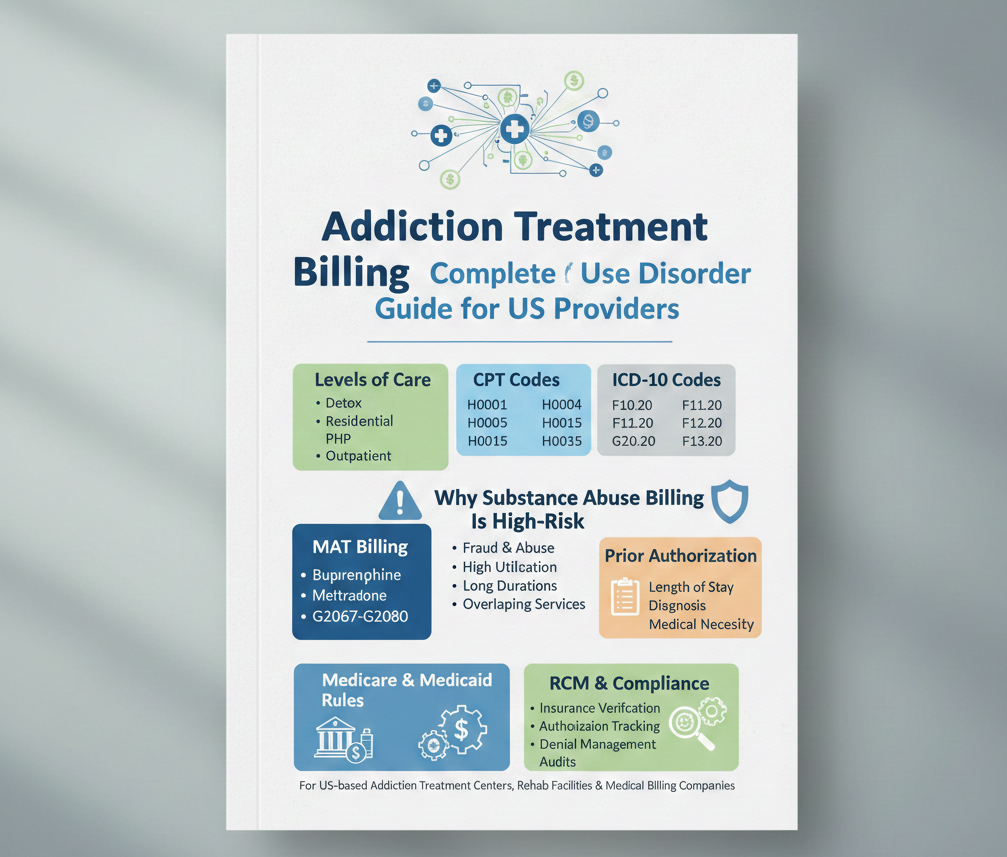
Levels of Care in Addiction Treatment Billing
Billing requirements depend heavily on the level of care provided.
Common Levels of Care
- Detoxification (Detox)
- Residential Treatment
- Partial Hospitalization Program (PHP)
- Intensive Outpatient Program (IOP)
- Outpatient Therapy
CPT Codes Used in Addiction Treatment Billing
Frequently Used Addiction Treatment CPT Codes
H0001 – Alcohol and drug assessment
H0004 – Individual substance abuse counseling
H0005 – Group counseling
H0015 – Intensive outpatient treatment
H0035 – Mental health partial hospitalization
Many of these codes are state-specific and commonly used by Medicaid and commercial payers.
Medication-Assisted Treatment (MAT) Billing
MAT is a cornerstone of modern addiction care and requires precise billing.
Common MAT Medications
- Buprenorphine
- Methadone
- Naltrexone (Vivitrol)
MAT Billing Codes
G2067–G2080 – Medicare MAT bundled services
J2315 – Naltrexone injection
MAT billing often includes drug administration, counseling and monitoring services.
ICD-10 Diagnosis Codes for Substance Use Disorders
ICD-10 codes establish medical necessity for addiction services.
Common SUD Diagnosis Codes
F10.20 – Alcohol dependence, uncomplicated
F11.20 – Opioid dependence, uncomplicated
F12.20 – Cannabis dependence
F13.20 – Sedative dependence
Prior Authorization in Addiction Billing
Most addiction treatment services require prior authorization.
Authorization typically depends on:
- Level of care
- Length of stay
- Diagnosis severity
- Medical necessity documentation
Medicare Rules for Addiction Treatment Billing
Medicare covers addiction treatment services under specific conditions.
Medicare Coverage Includes:
- Outpatient SUD treatment
- Opioid Treatment Programs (OTP)
- MAT services
Medicaid Addiction Treatment Billing
Medicaid is the largest payer for addiction treatment in the US.
Medicaid rules vary by state but often include:
- Daily or weekly billing limits
- State-specific HCPCS codes
- Mandatory treatment plans
- Frequent reauthorization
Billing teams must follow state Medicaid manuals carefully.
Common Modifiers in Addiction Billing
Modifiers clarify services provided.
HF – Substance abuse program
HK – Higher intensity services
59 – Distinct service
25 – Separate E/M visit
Documentation Requirements for Rehab Billing
Strong documentation is the backbone of addiction billing compliance.
Required records include:
- Intake assessments
- Treatment plans
- Progress notes
- Group therapy attendance
- Discharge summaries
RCM for Addiction Clinics
Addiction treatment billing performs best under a strong RCM framework.
RCM includes:
- Insurance verification
- Authorization tracking
- Accurate coding
- Claim submission
- Denial management
- Compliance audits
Outsourcing Addiction Treatment Billing Services
Benefits of Outsourcing
- Expertise in SUD regulations
- Reduced denials
- Faster reimbursement
- Compliance support
- Scalable billing operations
Compliance , Fraud , and Audit Risks
Addiction treatment billing is closely monitored by:
- CMS
- State Medicaid agencies
- Commercial insurers
- High-risk areas include:
- Length-of-stay billing
- Group therapy frequency
- MAT overutilization
Best Practices for Addiction Treatment Billing
- Verify benefits before admission
- Track authorizations daily
- Separate bundled and non-bundled services
- Use SUD-experienced coders
- Perform monthly compliance reviews
Closing statement
Addiction treatment billing requires specialized knowledge of substance use disorder coding, authorization workflows, MAT billing and payer compliance. For US rehab facilities, accurate billing is critical not only for reimbursement but also for long-term payer relationships.
By implementing strong billing systems or partnering with experienced addiction treatment billing services, providers can reduce denials, avoid audits and focus on delivering life-changing care.